Healthcare Compliance Perspective:
The recurring theme of fraud as a slippery slope is present in the following news story. The intentions behind committing fraud may start as a creative, yet illegal, way to make ends meet but have the potential to snowball into a case for 151 counts of healthcare fraud.
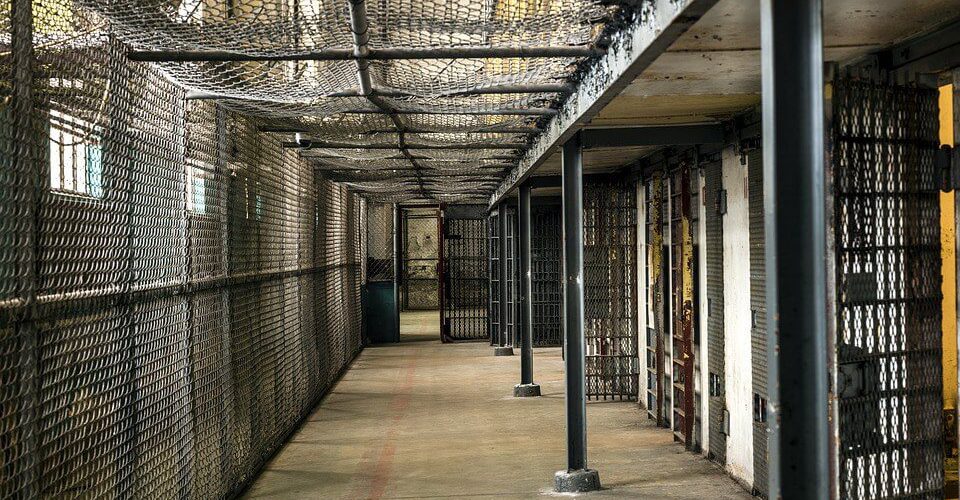
Oklahoma City, Oklahoma A U.S. States Attorney and Oklahoma’s Attorney general recently announced that a woman, and her son both of Oklahoma City, had been sentenced to prison by a United States District Judge for submitting false claims to Medicaid for behavioral health counseling to Medicaid-eligible children. Bot h defendants pled guilty on January 4, 2017, to one count of executing each of the three schemes. The woman, will serve 37 months and her son will serve 12 months and one day in federal prison. Both will serve three years of supervised release after imprisonment. The Court also ordered the pair to pay $769,578.38 in restitution to Medicaid.
h defendants pled guilty on January 4, 2017, to one count of executing each of the three schemes. The woman, will serve 37 months and her son will serve 12 months and one day in federal prison. Both will serve three years of supervised release after imprisonment. The Court also ordered the pair to pay $769,578.38 in restitution to Medicaid.
Claims were submitted to Medicaid for one-on-one “psychosocial rehabilitation services” that exceeded the billing maximum of 90 minutes per child per day, and they submitted Medicaid claims for one-on-one “psychosocial rehabilitation services” that were not actually provided, were actually provided in groups of two or more children, or were provided for less time than was billed to Medicaid
Compliance and Ethics Code of Conduct – Fraud and Abuse:
Contractors are expected to take necessary steps to prevent the submission of claims for payment and reimbursement of any kind that are fraudulent, abusive, inaccurate, or medically unnecessary.